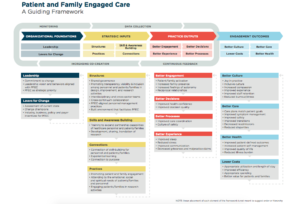
One element of the Guiding Framework that has always fascinated me is Engagement Outcomes as defined by culture, care, costs, and health. In looking at the PFEC Framework, measuring these engagement outcomes and gathering data is key, so the question is how do you measure engagement outcomes?
Oftentimes, hospital leaders looking to implement patient and family engagement strategies have challenges in collecting and analyzing data as it relates to the program. They are often left with anecdotal information seen via patient complaints or comments, or through one-off exchanges that make it difficult to quantify how these programs drive lasting and meaningful improvements. To ascertain the effectiveness of your strategies, it is important to gather quantitative feedback through real-time conversations with patients and their family members. These conversations should have the goal of uncovering what is important to them and enable immediate service recovery and resolution.
Collecting the Right Information for Patient and Family Engagement Strategies
For organizations looking to assess patient and family activation, one of the easiest ways to collect information is through other patient engagement programs. In fact, you could program the Patient Activation Measurement (PAM) tool into pre-arrival surveys, digital rounding scripts, kiosk assessments, or follow-up calls by asking patients or family members targeted questions before, during, or after the hospital stay.
This information, as Judith Hibbard suggests, would be used to inform the care plan. To assess whether the patient and family believe the relationship with the care team is reciprocal, you could ask them about the partnership in planning their care, making decisions and finding solutions. Additionally, technology can ensure patient’s safety post-discharge, a key metric that is unattainable if not asked directly. Lastly, by asking the patients about the adequacy of their sleep, their levels of stress related to care planning and medical decision-making or communication among the care team, we can determine how the experience is and do immediate service delivery if there are issues.
The Results of Implementing Effective Patient and Family Engagement Strategies
By asking the right questions during rounds or during post-discharge follow up, providers can identify opportunities for immediate service recovery and reassure the patient and family that we are effectively addressing their areas of concern. It is for this reason our solutions prove effective in reducing infection, decreasing falls, reducing readmission rates, and improving HCAHPS scores.
- Specifically, some of the results CipherHealth clients have seen include the following:
By proactively reaching out to patients within 24-48 hours of discharge, a large Indiana-based academic medical center saw a 20% reduction in readmissions for patients who engaged with their CipherOutreach Post-Discharge calls. Read the full case study. - With proactive leadership rounds focused on service recovery, a New Jersey-based hospital addressed patient needs prior to discharge and saw a 60% reduction in grievances and an average HCAHPS increase of 12.5% across domains. Read the full case study.
With customized questions, advisory support, and outcomes analysis, our technology is uniquely situated to assess the effectiveness of all your strategies. This is a valuable resource that can help showcase the importance of patient and family engaged care while providing qualitative and quantitative evidence to support ongoing initiatives.
Read more about the impact of technology on patient and family engaged care. If you are going to be at the Planetree Conference in Baltimore, please stop by booth #30 for more information about how technology can meet your patient and family engaged care goals.