The U.S. strategy for fighting COVID-19 has largely focused on preventing infection. While this defensive position was necessary, big issues facing population health—avoidable disparities leading to shorter life expectancy and higher rates of disease—continue to fester.
Population health in the U.S. was already compromised, and COVID-19 pushed it over the edge.
Late last year, an NPR poll found that 1 in 5 American families were delaying healthcare for serious illness. Currently, various utilization rates of routine preventative care—childhood immunizations or colon cancer screenings—have fallen sharply.
Hospitals continue to be under enormous strain, with delays and changes from normal care, as strapped providers try to do more with less.
Moreover, in non-crisis times, healthcare was too expensive or untrustworthy for many Americans and COVID-19 only exacerbated these disparities in health equity. In the U.S., people of color not only receive less care, but worse care.
The negative impact on the historically marginalized remains unaddressed.
The COVID-19 pandemic has shone light on long-standing structural and medical vulnerabilities in the U.S. healthcare system that impact historically marginalized groups the most. Minority populations have had higher rates of infection, hospitalization, and death.
Additionally, the most at-risk communities have taken the biggest economic hit during COVID-19, with hospitals in lower income areas losing millions of dollars because of fewer elective procedures and reallocation of resources.
There are no immediate solutions to these widespread problems. However, any approach to addressing them must appreciate the intersection between social and medical vulnerabilities.
Given this dire situation, how can automated tools help?
Given these social and medical inequities coupled with the unprecedented strain on the U.S. healthcare system after two years of COVID-19, how might technology—automated tools, such as digital outreach or rounding—alleviate some of the burden currently facing our hospitals, healthcare workers and patients in crisis?
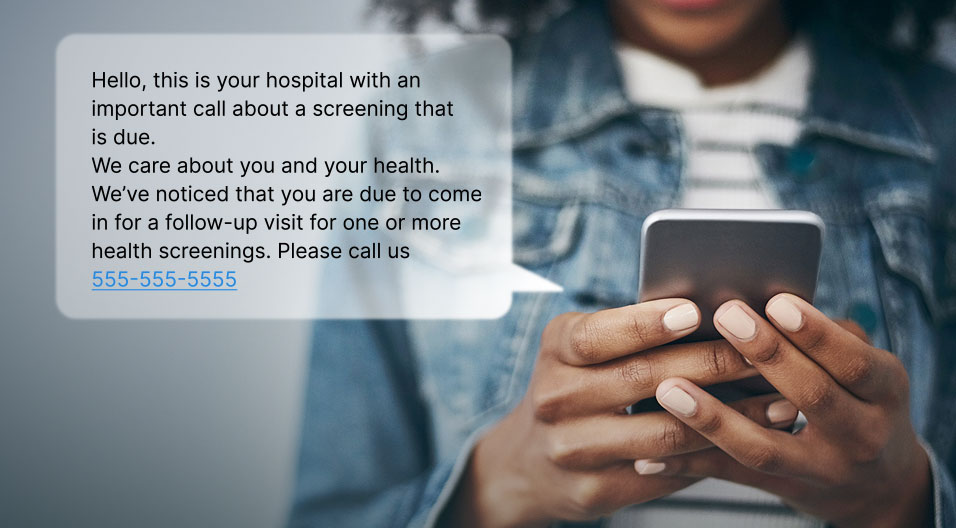
- Automated communication for expanded reach and education in your community. Employ digital outreach technologies to contact large populations with updates about COVID-19, vaccination reminders, annual wellness visits, care prevention, diabetes, flu prevention, mammograms, well-child visits, etc.
- Improved resource allocation and coordinated oversight. Take advantage of automated, pre-care communications before patients step into the hospital, saving thousands of hours annually for staff and increasing monetary value by ensuring that patients stay within your health system.
- Customized, patient-specific, condition-specific messaging beyond the hospital stay. Use post-discharge outreach to prevent readmissions by contacting all your patients, answering their questions and ensuring they are following their recommended care plans.
- Staff rounding to ensure effective communication, recognition and mental health support are being provided. Implement best practice rounding scripts to check in with every staff member to address personal or professional concerns and make certain they have the resources and support they need.
- Patient rounding to establish trust and understand any burning issues. Implement best practice rounding scripts to address immediate needs and any DEI concerns. Purposeful patient rounding can also help improve overall patient satisfaction, safety, quality of care, and clinical outcomes.
Technology creates opportunities for addressing pressing issues in population health.
The pandemic worsened long standing difficulties in population health initiatives and reaffirmed problems surrounding healthcare disparities we already knew existed. Employing technology to do even some of the heavy lifting potentially allows healthcare systems to reprioritize population health initiatives and improve communication in healthcare while continuing to address COVID-19. This approach to community health improvement translates into more effective engagement with vulnerable communities, improved health outcomes, coordination and more closed care gaps throughout patients’ care journey.