Contributors: Kamila Berkalieva, MPH; Jami Kelmenson; Alyssa Kleinman; Lyndsey Lord, M.B.A., R.N.; Aisha Qamar, MPH
ABSTRACT
Vulnerable patient populations such as those that are covered under Medicaid managed care face particular challenges in staying connected with healthcare providers. Studies have shown that engaged patients achieve better health outcomes, and as such, managed care organizations (MCOs) partner with hospitals and health systems to close care gaps and ensure patients follow the recommended steps of their care plans. This data analysis measured the impact of consistent telephonic engagement in encouraging patients to close care gaps and schedule their annual wellness visit. The results demonstrated that automated outreach can be an effective strategy in reaching and connecting patients to close gaps in care. The outbreak of COVID-19 has further demonstrated the need for patients to adhere to care plans and the importance of consistent patient/provider communication.
KEYWORDS
Care Gaps, Patient Engagement, Member Outreach, Patient Communication, Wellness Visits, Medicaid Members, Medicaid, Uninsured, Low-Utilizers, Non Utilizers, Self-Pay, Safety Net
INTRODUCTION
Closing gaps in care by promoting regular wellness visits contributes widely to improved quality and overall population health, with decreased costs. Historically, through programs like Healthcare Effectiveness and Data Information Set (HEDIS) and Patient-Centered Medical Home (PCMH), the Centers for Medicare & Medicaid Services (CMS) and the National Committee for Quality Assurance (NCQA) have linked reimbursement (or penalties) for healthcare services to patient outcomes.
Patient engagement is a key contributor toward successful HEDIS scores and PCMH recognition. Especially in these fragile times fraught with concerns over states reopening too quickly, patient engagement becomes even more crucial in minimizing the impact of deferred care and other challenges posed by the COVID-19 crisis. The benefits of closing care gaps as we move through phases of the COVID-19 pandemic are to help drive essential patient loyalty, improve follow up, and achieve better population health outcomes.
CHALLENGES IN ENGAGING SAFETY-NET POPULATIONS
The largest public health system in the nation provides essential inpatient, outpatient, and home-based services to more than one million New Yorkers every year in 70 locations across the city’s five boroughs. In serving safety-net populations, this health system found it challenging to engage patients in completing their annual wellness visits and adhering to their plan of care. Particular barriers facing these patients, such as unstable housing, and missing or incorrect phone numbers, make it difficult to connect with them. As a result, the health system faced challenges reaching and serving Medicaid patients in a timely way.
In addition to the barriers this population faces, the manual process followed by their team was disparate, time-consuming, and difficult to scale for a larger population. To more efficiently close care gaps, their team needed to streamline this workflow across facilities, reengage patients in their care, and close care gaps for high-risk patients to prevent negative outcomes an inappropriate utilization. Efficient and consistent outreach with the flexibility to scale as the organization’s needs evolved was key to achieving these goals.
ENGAGEMENT PROCESS
Using data analytics and hospital registries, CipherHealth was able to help this health system identify and reach patients in need of scheduling an appointment. CipherHealth implemented a program in which automated calls went out to nearly 170,000 patients, the majority of whom hadn’t seen their PCP in more than 12 months. Patients received educational reminders for their annual wellness visits. Subsequently, patients who wished to schedule a preventive screening or other care were connected to a non-clinical call center representative to assist with making an appointment based in the borough in which they live.
The outreach program included a series of automated calls with messaging encouraging the patient to schedule his or her annual wellness visit. CipherHealth received lists from the health system of patients who were due for their annual visit each month. These patients were then enrolled in the outreach call program. To meet the needs of this patient population, calls were conducted in eight languages: English, Spanish, Mandarin, Cantonese, Haitian Creole, Bengali, Russian, and Polish.
Once patients engaged with the call and indicated they would like to schedule an appointment, the appropriate follow up was completed by operators at borough based call centers who assisted with scheduling primary care appointments.
PROGRAM RESULTS
CipherHealth and this health system conducted a retrospective analysis using data for ~170,000 patients to measure the effectiveness of consistent automated outreach on getting patients to schedule annual wellness visits. The study population was comprised of individuals who were due for their regular annual wellness exam between February 1, 2018 – December31, 2019.
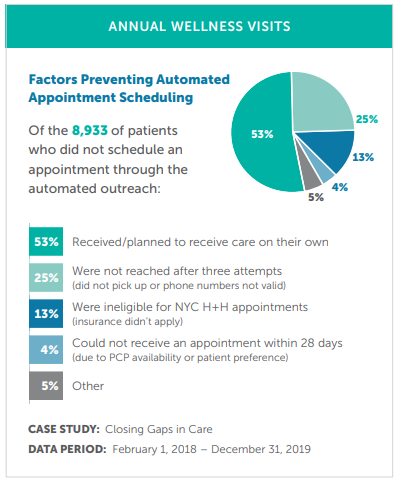
Twenty percent of eligible patients engaged with the call. Of these, 38% (n = 13,189) requested assistance scheduling an appointment, 32% (n = 4,256) of which then scheduled an appointment via a call back from a borough call center representative. The chart to the right offers some data points as to why patients might not have scheduled an appointment through the automated system. For example, 53% received or planned to receive care on their own, so it’s possible the call still triggered the desired action on their part.
The health system significantly exceeded its communications goal for engaging this hard-to-reach population using CipherHealth’s automated outreach technology. In addition, they were able to gain actionable insights into this population, including patients’ language preferences, a key data point that will help them better serve the community in the short- and long-term. The health system has since expanded the number of eligible individuals to receive a call through this program from 170,000 to 500,000 patients/year.
CONCLUSION
This study suggests that consistent engagement with patients promotes compliance with scheduling annual wellness visits. The automated calls allow patients multiple opportunities to communicate needs while providing the health system with the information and workflows necessary to help address patient concerns quickly. Further, even if patients do not pick up or engage with the call, it could act as a prompt for them to still take action on their own to schedule their wellness visits. By partnering with CipherHealth, the largest public health system in the U.S. ensures all eligible patients receive preventive health outreach to close gaps in care — at a time in our history when it’s never been more important to do so.