The transition of care from hospital to home is the last opportunity a health system has to confirm that patients understand their care. Ensuring that patients adhere to personalized care plans during the recovery process has proven to reduce readmissions significantly. For nurses focused on their inpatient population, however, finding the time to call discharged patients can prove challenging.
Located in Pompton Plains, New Jersey, Atlantic Health System-Chilton Medical Center is a 260-bed, fully accredited acute care hospital. Recently, the organization has implemented a number of initiatives to ensure patients understand and adhere to important care information post-discharge. By regularly communicating with patients through inpatient rounding and post-discharge follow-up calls, nurses at Chilton are creating positive touch points throughout the care continuum. At the same time, Chilton is leveraging key pieces of information to stay up-to-date on its patient populations’ needs. Checking in with patients not only assists with their overall care and recovery, but also helps prevent readmissions to the hospital. This is of utmost importance in today’s hospital payment landscape due to financial penalties that can accrue based upon readmission rates.
Challenge
Ideally, a health system follows up with 100% of patients to see how they are faring at home and address any questions about symptoms, discharge instructions, or medications. This process allows providers to identify patients at risk for readmission and to intervene before an adverse event occurs. Often, a patient has questions or concerns that can be resolved preemptively, preventing the need for readmission; however, providers often lack the necessary time and resources to identify and address these issues properly.
Nurses typically have onerous workloads and time constraints before factoring in follow-up calls making it nearly impossible to follow up with each patient. Follow-up calls are often the first thing eliminated from a nurse’s daily schedule so that he or she can attend to the needs of patients in the hospital.
After considering the proven benefits of post-discharge follow up, Chilton implemented various workflows and initiatives to call discharged patients. The staff quickly found that manually calling every patient was difficult to sustain. They also lacked effective data collection methods to inform hospital administrators of the root causes for readmissions. Instead of relying on paper-based surveys, the hospital sought out a scalable solution that would reach out to 100% of discharged patients, while also collecting and analyzing data to drive further outcome and experience based improvements.
Solution
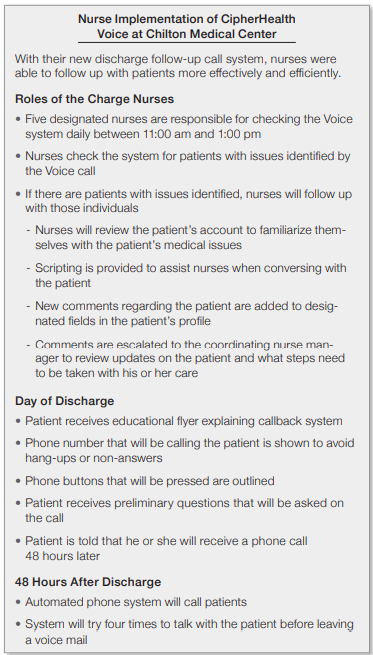
With other Atlantic Health System sites having partnered with CipherHealth, Chilton saw the benefit in implementing the company’s follow-up call platform, Voice, to assist with its facility-specific quandaries.
Chilton found that compared to an all manual program, Voice reached more patients, more consistently after discharge. On the Voice calls, patients answer a series of questions designed to track their recovery progress at home and also give feedback on the inpatient experience. If a patient indicates a clinical or service issue on the Voice call, a provider is immediately alerted and follows up with the patient within 48 hours. This feature enables quick issue resolution and intervention before an adverse event occurs. The calling platform features messages recorded in the friendly and familiar voices of nurses at Chilton, allowing the facility to maintain its personal approach to post-discharge follow up.
“We are trying to make the patient experience as personable as possible,” says Tania Cutone, Nursing Manager and Informaticist at Chilton. “Rather than using a robotic automated recording, this platform allows patients to hear the voice of a staff member who had assisted them throughout their care experiences.”
To enhance standardization across sites, Chilton’s follow-up call scripts utilize the best-practice questions used by other Atlantic Health System facilities. This list of questions was co-developed with CipherHealth to best reach the system’s unique patient population.
Chilton was also able to customize Voice’s reporting and analytics features to incorporate unique reports. The facility worked with CipherHealth to integrate Voice into its existing scores reporting methodology, so that its patient satisfaction manager could link all of Atlantic Health System’s reporting systems together. With organization-specific features now integrated within Chilton’s Voice platform, satisfaction scores could be documented and pulled into a database where feedback and reports could be monitored in real time. This ensured that follow-up calls would provide data helpful not only for reducing readmissions, but also for improving the entire patient experience.
“CipherHealth has been extremely responsive whenever we have had requests regarding their products,” Cutone says. “They were more than willing and open to work with our specific needs.”
Results
With the personalized system in place and through the assistance of CipherHealth administrators, Cutone was able to begin conducting training seminars and pilot programs to demonstrate the use of the product. Due to its ease of use, instructions for utilizing the product were quickly adopted by staff members.
In all, Voice dramatically helped with the upkeep of post-discharge calls. No longer burdened with backlogged call schedules, nurses were able to ensure that the specific patients requiring high-touch post-discharge interventions received a call within 48 hours and were able to address any issues before an adverse event occurred. Additionally, Voice keeps records of all call information, ensuring that patients are receiving pertinent information and tracking data to identify trends that help Chilton drive further improvements.
Nurses can now spend more time on the floor with patients and less time with administrative tasks, something Cutone indicated as being one of the largest benefits realized by the program.
“Nurses are a lot happier now because they used to spend a lot of time trying to call 100% of their patients,” Cutone says. “Voice now affords them more time on the floor to provide better care for individuals and limits delayed calls.”
Using Voice has allowed Chilton to effectively monitor and assess the care needs of its patient population by reducing the amount of time spent making daily follow-up calls. This dynamic partnership between Atlantic Health System-Chilton Medical Center and CipherHealth has enabled nurses to provide superior care to patients throughout the care continuum.