Collaboration between the care team, the patient, and their care provider is essential for developing a personalized plan of care and an effective care transition plan that aligns with the patient’s preferences and needs. This partnership ensures that the care plan is patient-centered, promoting better adherence to treatment and improving health outcomes. Engaging the patient and their provider fosters open communication, allowing the care team to gain valuable insights into the patient’s goals, cultural values, and social determinants of health. Additionally, it builds trust, empowers the patient to take an active role in their care, and reduces the risk of misunderstandings or gaps in care during transitions. By working together, the care team can create a seamless, coordinated approach that supports the patient’s overall well-being.
Key types of communication include: :
- Patient-Provider Communication ensures that patients understand their diagnoses, treatments, and care plans. It involves clear explanations, active listening, empathy, and making time for patients to ask questions and express concerns.
- Multidisciplinary Communication refers to the exchange of information and communication across providers and healthcare professionals (e.g., doctors, nurses, pharmacists, therapists) to coordinate care, discuss patient status, and develop care plans.
- Family and Caregiver Communication engages patients’ families or caregivers in discussions about plan of care, prognosis, and next steps. This ensures that the patient’s support network is informed and aligned with the healthcare goals.
- Cultural and Linguistic Sensitivity that adapts communication to the patient’s cultural background, language preferences, and literacy levels to promote understanding and avoid miscommunication.
- Non-verbal Communication encompasses body language, facial expressions, and tone of voice, which can complement or contradict spoken words. In healthcare, these non-verbal cues are crucial in fostering trust and enhancing understanding between patients and providers.
Together, these forms of communication across healthcare settings enhance patient outcomes, minimize medical errors, decrease unnecessary patient and family anxiety, boost patient satisfaction, and foster trust in the healthcare system.
Why is Communication Important in Healthcare?
Communication is vital in healthcare because it ensures accurate information exchange between providers, patients, and their families, which is essential for delivering safe, high-quality care. Effective communication helps healthcare teams coordinate seamlessly, reduces the likelihood of medical errors, and improves patient outcomes. For patients, clear communication builds trust, enhances satisfaction, and empowers them to participate actively in their care. It also supports the development of personalized care plans that align with the patient’s preferences, cultural values, and needs, promoting better adherence to treatment and overall well-being.
Effective communication of healthcare information can empower patients and their family members to participate as full partners in their care, and is demonstrated to improve adherence to treatment and self-management.
Moreover, a structured approach to health communication can measurably improve healthcare delivery.
The importance of patient-provider communication extends far beyond the inpatient setting. When patients are no longer under the care of healthcare professionals, care teams should continue to communicate with patients via various modalities to ensure safe outcomes and strengthen meaningful relationships with care providers.
Effective Communication in Healthcare is Crucial for Ensuring Safe Care Transitions
Care transitions from one healthcare setting to another are critical times for patients and families.
Whether it’s transitioning from acute care to home or moving from wellness care to chronic disease management, these moments are full of opportunities where key aspects of healthcare communication can be missed, impacting patient outcomes, loyalty, and satisfaction.
Think about a time when you’ve had to manage a care transition of patient care on your own or as a caregiver for a loved one. t These are times of elevated anxiety and heightened concern about what to expect.
From a health communication perspective, these are moments when crucial healthcare information may fail to be transferred properly, be misunderstood, or be dismissed by the patient and family because they do not fully understand the importance of the information being discussed.

Why is Communication Important in Health and Social Care?
In addition to the amount of health information a patient and family are challenged to absorb regarding new medications, follow-up care, possible physical therapy required, and clinical symptoms, Social determinants of health (SDOH) can significantly impact a patient’s recovery and overall well-being after being discharged from the hospital. These factors include economic stability, access to healthcare, education, social support, neighborhood environment, and employment status.
After discharge, SDOH can influence a patient’s ability to adhere to treatment plans, access necessary medications, and follow up with healthcare appointments. For example, patients with limited financial resources may struggle to afford prescriptions or transportation to follow-up visits, while those lacking strong social support may experience isolation, which can hinder their recovery.
Poor housing conditions, lack of access to healthy food, or unsafe environments may also exacerbate existing health conditions, leading to readmissions or poor long-term health outcomes. Addressing these factors is critical for improving patient recovery, reducing readmission rates, and ensuring sustained health improvement.
SDOH and health literacy are well-documented issues that can affect recovery following an inpatient stay.
Furthermore, changes in reimbursement have led to decreased Length of Stay (LOS), which may also impact patients’ time to digest and understand the care plan before moving to their next healthcare setting.
Healthcare systems are being held accountable for delivering high-quality, cost-effective care through value-based care models and performance-based incentives.
These models focus on the outcomes of care rather than the volume of services provided, encouraging hospitals to prioritize patient satisfaction, safety, and overall health improvement while controlling costs. Insurers track key metrics such as readmission rates, patient outcomes, and adherence to clinical guidelines, offering financial rewards for hospitals that meet or exceed benchmarks.
Conversely, hospitals that fail to meet these standards may face penalties or reduced reimbursement rates. This approach incentivizes hospitals to implement more efficient care processes, reduce unnecessary treatments, and improve patient care coordination, ultimately leading to better outcomes for patients and cost savings for the healthcare system.
With this pressure on healthcare systems, effective communication around discharge planning must begin upon admission to the hospital. When discharge planning begins early, it allows the care team to assess a patient’s needs, coordinate services, and ensure a smooth care transition from the hospital to home or other care settings.
Clear communication helps align expectations between patients, families, and healthcare providers, ensuring that patients are well-prepared for discharge, understand their care instructions, and have the necessary resources in place for recovery.
This proactive approach can reduce the risk of complications, prevent unnecessary readmissions, and optimize the length of stay without compromising the quality of care. By addressing discharge planning early, healthcare systems can improve patient outcomes, enhance satisfaction, and meet goals for efficiency and cost-effectiveness.

Effective Communication in Discharge Planning
Hospital discharge especially can present a significant challenge for patients and their loved ones.
Discharge planning is inherently complex, as providers must gather and communicate information tailored to the patient’s functional status, expressed preferences, and follow-up care instructions.
Often, busy clinicians are forced to rush through discharge education and instructions, which can negatively impact the patient’s comprehension and thus, adherence to the plan of care.
Although patients may be more comfortable at home with the support of family and friends and away from the stresses of a hospital or post-acute setting, for some, this transition becomes challenging and may result in critical gaps in patient care.
Prepare Patients for the Transition from Hospital to Home Care
To prepare patients for safe transitions from hospital to home, many leading health systems have targeted workflows and teach-back methods designed to improve communication during this potentially vulnerable time for patients.
One of the most t effective strategies is pairing two communications: the transitional care round and post-discharge outreach call.

Transitional Care Round
The transitional care round consists of a final review of the personalized discharge plan, including home care needs, durable medical equipment, transportation, patient safety information, follow-up appointments, care instructions, and signs and symptoms to monitor.
Verbal communication such as asking permission to sit down next to the patient and pulling the chair close to the bedside can also have a positive effect—studies show that patients perceive a provider has spent more time with them when they sit rather than stand.
Patient perceptions of their care are very much informed by the quality of their verbal communication skills with their nurses, clinicians, and every healthcare provider they come in contact with. They will remember the attention, kindness, and respect they received from the healthcare team.
Post-Discharge Outreach Call
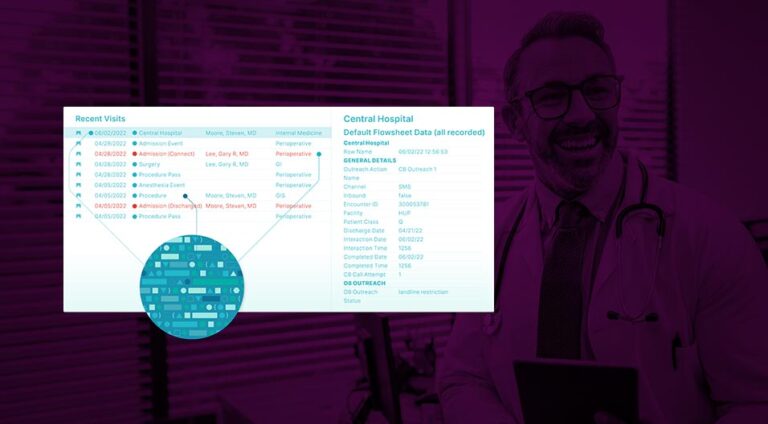
It’s also critical that health systems establish a consistent communication strategy for the automated process of the post-discharge outreach calls.
The post-discharge outreach call confirms that this plan has been effectively carried out and assesses if the patient has remaining questions for healthcare professionals that can be immediately addressed.
In order to make the transitional care round purposeful, clinicians and nurses need to take the time for heartfelt, relaxed, and unhurried interactions with patients that do not follow a tight script.
To ensure patients stay on the path to recovery, clinicians and nurses should follow up with all patients and provide the opportunity to request help and guidance from healthcare providers.
Before discharge, healthcare providers should explain to patients that they will receive automated calls as part of their transitional care and let them know a nurse will be available if they need assistance. This personal touch increases the chance that patients will answer the call.
By proactively communicating and engaging with patients following discharge, healthcare providers can better equip patients to care for themselves – leading to improved patient outcomes, increased patient satisfaction, and reduced readmissions.
Healthcare Communication in Action
CipherHealth analyzed the effectiveness of implementing these complementary communication strategies in a retrospective data analysis of 77 customers, including 484 hospitals and 84,570 patients, over the course of 24 months.
For patients who received a transitional care round prior to discharge, 4.51% flagged confusion over discharge instructions during the outreach call, compared to 7.25% who did not receive a transitional care round.
In other words, a lack of transitional care round was correlated with a greater likelihood of patients not understanding their discharge instructions and needing assistance after returning home.
Patients who received a transitional care round were also more likely to complete the post-discharge outreach call.
In another study measuring the effectiveness of post-discharge outreach calls, CipherHealth found that patients who completed the post-discharge outreach call were readmitted 56% less often.
The True Importance of Communication in Healthcare: The Profound Impact on Patients
Trust is a high value currency in healthcare. Patients who do not trust healthcare organizations are far less likely to share critical information – medical and non-medical – that could play a key role in their health. And patient trust is built through impressions and micro-encounters outside of strict clinical encounters.
By providing tailored and timely communications, healthcare leaders can not only build trust, they can find opportunities to better care for the patient.
The bottom line is that a hospital visit can be distressing for both patients and their families. Patients may feel intimidated or hesitant to ask questions or seek more information, especially when dealing with a loss of functionality that often leaves them feeling a lack of control.
Healthcare leaders have the opportunity to preserve the dignity of patients in the face of illness and uncertainty through patient-centered communication. To meet patients in their moment of need, communication structures must extend far beyond the four walls of the healthcare facility to reflect the complexity of today’s healthcare journey.
Good communication methods are vital to dignified care – and patients deserve nothing less.
What are Strategies to Improve Communication in Healthcare?
1. Leverage Technology
Technology can be leveraged to improve communication with telemedicine and secure messaging systems allowing for ongoing interactions between patients and providers.
These digital patient-provider communications are especially useful for follow-ups, reminders, or answering patients’ questions outside of in-person visits.
2. Implement Structured Communication Tools
Implementing structured communication tools like SBAR (Situation-Background-Assessment-Recommendation) provide a standardized framework to ensure that essential information is passed clearly and efficiently, especially during patient handoffs. CipherHealth’s rounding tool can also serve as a guided reminder of key questions to ask during rounds, supporting High Reliability principles by promoting consistent and effective communication.
3. Enhance Active Listening
Medical professionals should practice active listening, giving full attention to patients or healthcare team members, asking clarifying questions, and repeating information to ensure understanding. This builds rapport and ensures information is accurately conveyed.
4. Encourage Interdisciplinary Collaboration
Another key strategy is to encourage interdisciplinary collaboration by fostering open communication between different healthcare professionals. Regular interdisciplinary team meetings or case reviews can be organized to improve coordination and reduce silos.
5. Cultural Competency Training
Cultural competency training is also necessary to enhance communication, as it helps healthcare providers understand and respect cultural differences, leading to more meaningful interactions with patients.
6. Teach Interpersonal Communication Skills
Medical staff should seek out training to improve their communication skills, especially in situations where they need to deliver difficult news, explain complex medical terms, or resolve conflicts.
7. Simplify Medical Jargon
To ensure better patient understanding, healthcare providers should avoid complex medical jargon and use plain language when discussing diagnosis or treatment plans.
8. Improve Patient Handoffs
Standardize and carefully manage the transfer of patient care from one provider to another, whether during shift changes or hospital transfers. Using structured handoff processes reduces information loss and ensures continuity of care.
9. Provide Patient Education
Another important strategy is to provide patients and their families with educational resources about their conditions and treatments, whether through printed materials, videos, or other decision aids. Visual aids such as diagrams and illustrations are particularly helpful in explaining complex information to patients with low health literacy. Additionally, care recordings are a valuable tool, allowing patients to replay their instructions at home to ensure they understand their care plan fully.
10. Utilize Non-verbal Communication
In terms of non-verbal communication, health professionals should be mindful of their body language, facial expressions, and tone of voice, as these cues can significantly impact how patients perceive their care.
11. Encourage Open Feedback
Fostering an environment that encourages open feedback from both patients and healthcare staff allows for continuous improvement in honest communication practices.
12. Adopt Language Interpretation Services
For patients with limited English proficiency, ensure access to professional interpreters (either in-person or through remote services) rather than relying on family members to bridge the language barrier, which can lead to miscommunication.
13. Create a Supportive Environment
Cultivate an environment where medical staff feel comfortable speaking up about concerns or questions, especially when patient safety is at risk. This promotes a culture of transparency and collaboration.
14. Use Visual Aids
Diagrams, charts, and illustrations can help patients better understand their conditions or treatments. This is particularly effective for patients with low health literacy or those who learn better visually.
Implementing these strategies can significantly enhance communication among healthcare providers, patients, and their families, ultimately leading to improved patient care and outcomes.