The following article originally appeared in Becker’s Hospital Review.
Patient engagement has become a popular term utilized throughout the healthcare industry, and for good reason. As value-based care models mature and new payment models focus on quality over quantity, keeping patients engaged is an effective way of reducing the overall cost of care, improving outcomes, and increasing patient satisfaction.
However, many providers are still asking, “What does patient engagement mean and how can healthcare organizations get ahead of the curve?”
In a recent webinar, CipherHealth explored both the definition of an effective patient engagement strategy and a related maturity model, as well as ways in which an organization can get started and continuously improve maturity. Lisa Romano, MSN, RN, CipherHealth CNO, kicked off the webinar by discussing the new patient engagement model that extends beyond the “four walls” of a hospital to meet patients where they are during their care journey. To demonstrate this new model in action, Joyce Komori, MSN, RN, AVP of Care Management at Providence St. Joseph Health – SoCal, shared how St. Joseph Heritage Healthcare is leveraging patient outreach as the cornerstone of a comprehensive patient engagement strategy.
Exploring the New Patient Engagement Model
Lisa Romano begins the webinar by describing the fundamental differences between patient engagement and patient experience. She states, “Patient engagement is the strategy that healthcare organizations and other providers undertake to optimize the patient experience across the continuum of care. Patient experience, as defined by the Beryl Institute, is the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.
According to a survey by Modern Healthcare of over 200 healthcare leaders, among the components of a successful patient engagement program are appointment scheduling/reminders, patient rounding, care management, and preventive health outreach. Though each of these components is important, post-discharge follow-up is seen as the number one indicator of a successful patient engagement program.
Because the patient journey is no longer linear and may include multiple trips to a hospital, physician office, or other health facilities, the need to continuously engage a patient along the care continuum has become increasingly important – yet also more difficult. Like other long-term initiatives, healthcare organizations are in different stages of maturity in regard to their patient engagement strategy – and those that are further along in their journey derive significant advantages from their ability to proactively engage with patients to create a cohesive experience across the care continuum.
Lisa Romano introduces the new model for patient engagement by describing three levels of organizational maturity in how patient engagement is viewed and acted upon:
- 1.
Foundational level of maturity
- : Organization will measure HCAHPS scores as a primary driver
- 2.
Intermediate level of maturity
- : Organization will emphasize and focus on transitional care and outreach
- 3.
Innovative level of maturity
- : Organization will implement an integrated care experience across care settings
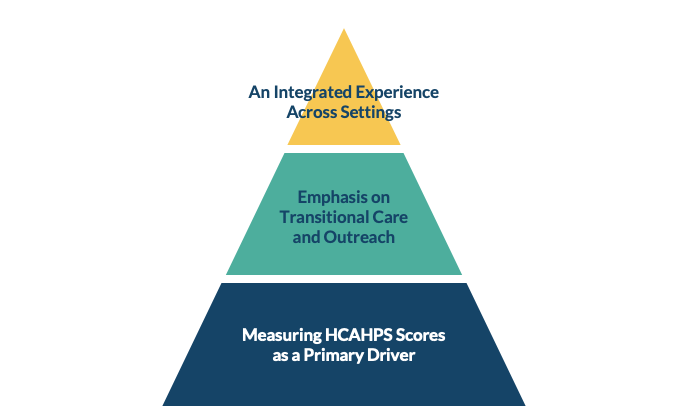
Model A: The New Model for Patient Engagement
Regardless of maturity level, healthcare organizations should leverage data to drive continuous improvement in the quality and experience of care delivery. As Lisa Romano recalls, “In my background as a hospital administrator, I needed data to justify [programs], to show trends. If I didn’t have data, it was very difficult to move any program forward.” Using her experience as an example, Lisa discusses how data can empower organizations to better engage with patients through actionable insights.
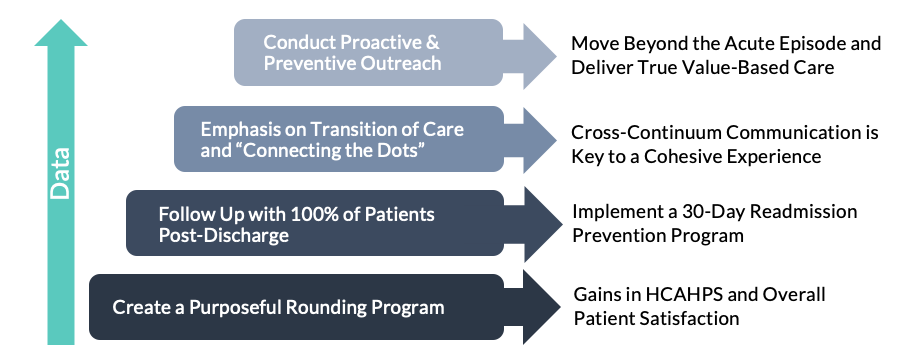
Model B: Steps to Take to Move Up in Patient Engagement Maturity
Improving Care Transitions for High-Risk Populations
One health system that engages patients at an innovative maturity level is St. Joseph Heritage Healthcare. Part of Providence St. Joseph Health, St. Joseph Heritage Healthcare (Heritage) was founded in 1994 and includes eight medical groups and supports six distinct affiliated physician networks throughout California.
As VP of Care Management at St. Joseph Heritage Healthcare, Joyce Komori manages all care management activities in Southern California, including the Discharge Follow Up Program (DCFU). The DCFU is part of a greater care management construct whose collective goal is to reduce readmissions and unnecessary utilization of services. Using this construct, the DCFU is alerted of high-risk patients that fall within the 5 hospitals that the DCFU supports in Orange County and High Desert, and high-risk patients that reside in the greater LA area. In 2018, the DCFU implemented CipherOutreach, CipherHealth’s automated outreach technology, to scale their outreach processes and achieve better patient outcomes.
Using a centralized ambulatory care management team in Brea, CA, the DFCU oversees all automated CipherOutreach calls for high-risk patients and manual post-hospital discharge follow-up calls for disease-specific populations.
From June 2018 through December 2018, Heritage reached 76% (7,743) of its target population using CipherOutreach. Within this same six month timeframe, patients that were reached with the automated outreach call had readmission rates that were 16% lower than those that did not interact with the call. What makes this program so successful? A few key elements of this program have led to its success:
- The automated outreach call has a local area code and unique Caller ID
- Nurses at the bedside and care managers at the hospital educate the patient about the purpose of the call and the questions that will be asked on the call prior to discharge
- If a patient requests a callback, the DCFU team will attempt to call the patient back within 5 minutes of that patient ending the automated call
CipherOutreach is a key strategy that Heritage utilizes to engage its high-risk and disease-specific populations. Through its multi-pronged longitudinal care management approach, including CipherOutreach and other programs, the organization has achieved significant cost savings. Within a 6-month timeframe, St. Joseph Heritage Healthcare found that patients that engaged with a longitudinal care management program had a 50% lower PMPM hospital cost than those that declined participation in the program.
In looking at where Heritage falls in the patient engagement model outlined above, one can see that Joyce and her team have created an integrated experience across care settings to accommodate the needs of each patient in his or her unique care journey. Heritage uses the trends and insights identified in CipherHealth’s pushed reports, Insights dashboards, and outcomes analysis to make improvements to its program on a bi-annual basis. Looking ahead, the team has met extensively to review data from the call and is excited to update the call script so that it generates an even higher reach rate and lower readmission rate.
As healthcare organizations continue to develop strategies that align with changing regulations and patient preferences, developing a comprehensive patient engagement strategy that engages patients during their hospital stay and throughout their care journey will be key. As Joyce recalls, “When we designed this program, we partnered closely with our health system quality team, our hospitals, our inpatient case managers, our nurses at the bedside, our ambulatory care management team, and our call center team to make sure we were really moving forward as one cohesive unit.” As Lisa and Joyce show, there are many strategies to drive better patient engagement, but the ultimate key to success will be partnerships built along the continuum of care to keep patients healthy and happy.
To learn more about how leading healthcare organizations leverage CipherHealth’s patient engagement platform to transform the future of care delivery, check out the following articles: