For too many patients, the rising cost of prescriptions creates a difficult choice—pay for essential medications or cover other basic needs.
In fact, according to a survey by the Kaiser Family Foundation (2024), approximately 25% of adults find it difficult to afford their prescription drugs, with larger shares among those who take more medications.
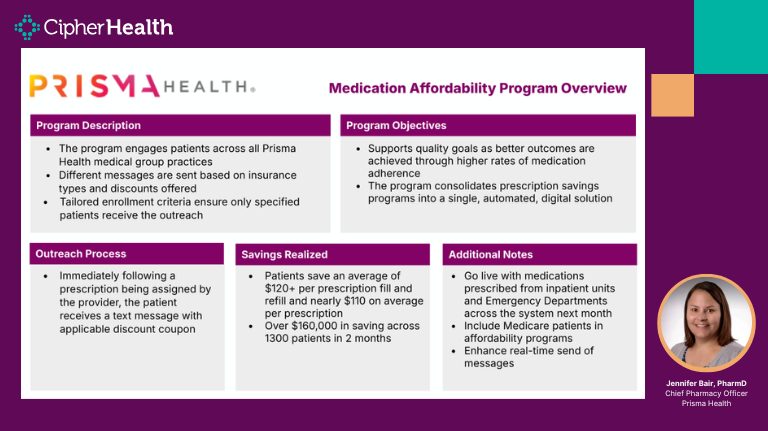
We had the chance to chat with Jennifer Bair, PharmD, Chief Pharmacy Officer at Prisma Health to dive into how the organization is leveraging CipherOutreach to automate and ensure more patients can afford their medication without financial stress.
Prisma Health is a private, nonprofit health system and the largest healthcare organization in South Carolina and Tennessee, serving 1.5 million patients annually.
Here’s how Prisma is transforming their approach to medication affordability.
Doing Away with Manual Processes
During the webinar, Bair highlighted the challenges Prisma Health faces in ensuring medication access for its patients, particularly those who are uninsured or underinsured.
“For geographical reasons as well as financial reasons, medication access, particularly with the rising costs, is something that we continuously struggle with for patients,” Bair said.
Before implementing CipherOutreach, Prisma Health relied on manual processes to connect patients with medication assistance programs.
“Last fiscal year, our medication assistance team served and provided just over $71 million worth of medication assistance to patients. But it was all through manual processes,” Bair noted.
These referrals depended on case managers, nurses, and pharmacists identifying patients in need—a system that, while effective, lacked consistency and scalability.
“We’ve tried working on other solutions to find ways to automate this, and we haven’t found any good solutions until starting to actually work with this one,” she said.
A Phased Approach to Expanding Access
Understanding the complexity of rolling out a system-wide change, Prisma Health took a measured, three-phase approach:
Phase One:
Prisma Health began with five select practices where internal champions could help identify and resolve issues before scaling up to additional locations. “We picked practices that we knew we had champions within that practice who would help us troubleshoot any issues,” Bair shared. This allowed the team to refine messaging and workflows before scaling up.
Phase Two:
With lessons learned from the pilot, Prisma expanded the program to include all primary care practices.
Phase Three:
The final phase will include specialty practices, bringing the program to full implementation across Prisma’s ambulatory network.
Key Considerations for Engaging the Right Patients
One key decision was setting exclusion criteria to ensure outreach targeted the right patients.
“We chose not to send messages to patients who were using our internal pharmacies because our medication assistance team was already supporting those patients,” Bair said.
Prisma Health also initially excluded Medicare patients to prevent any issues with out-of-pocket maximums and ensure compliance with insurance requirements.
“We wanted to make sure that we were intentional about when we included Medicare into the solution,” she said.
Given Medicare’s unique regulations on copay cards and discount programs, Prisma Health focused on providing clear guidance.
“One of the main messages that we have for patients is to talk to your pharmacist, which may be helpful to you, but understand your benefit and your out-of-pocket maximum before you use this card,” Bair said.
Now, Prisma Health is preparing to expand the program to Medicare patients, with carefully crafted messages to help them maximize their benefits without unintended financial consequences.
Fine-Tuning Messaging for Better Patient Engagement
CipherHealth supported Prisma Health to optimize its messaging for patients.
“We designed messages that were very specific, based on the type of insurance and the type of offer… The Cipher team has been really great in helping us get those messages just right,” Bair shared.
This collaboration ensured that patient communications were clear, relevant, and effective in addressing affordability concerns.
By delivering the right message to the right patient, Prisma Health is able to improve patient engagement, leading to higher response rates and greater program success.
Creating Meaningful Cost Savings
Since launching in October, the program has sent over 150,000 text messages with prescription savings opportunities.
The response has been overwhelmingly positive, with only 170 patients opting out. “To me, that is just really impressive. It really speaks to the fact that these patients are receiving this program very positively,” Bair said.
Beyond engagement, the financial impact for patients has been significant. “We are saving patients in total about $120, and per prescription, about $112,” Bair said.
High-cost medications, particularly GLP-1 drugs, have been among the most commonly used savings offers, reflecting the growing need for affordability solutions in chronic disease management.
Through automation, Prisma Health is breaking down barriers to medication access while ensuring a seamless experience for both patients and providers.
“We’re seeing a lot of success and a lot of good uptake from our patients,” Bair said.
That’s exactly why we’re here at CipherHealth. If you’re interested in making medication affordability a reality in your health system, reach out to us.