In this series, we explore the concept of Patient Experience as an outcome measure and Patient Engagement as the Strategy that healthcare organizations and providers take to positively impact the Patient Experience. In this article, we showcase how hospitals can leverage patient engagement to improve the care transition experience.
As we have discussed, engaging patients is a critical component of improving the patient experience. The key is to identify strategies that engage patients throughout their entire care journey to impact more than just patient satisfaction scores. One of the most important, but challenging, aspects of a patient’s journey is the transition process from one care setting to another.
During this time patients are often inundated with information and even the most thoughtful efforts to ensure they remember as much as possible may not be enough. Considering the impact of Social Determinants of Health (SDH) and clinical stresses that patients may still be experiencing at the point of discharge is key. One brief touch point with discharge instructions is not sufficient. The opportunity exists to record discharge instructions that can be accessed after discharge when they are more able to comprehend as well as supplement with a follow-up phone call giving the patient the opportunity to ask questions or request assistance with medications and follow-up doctor appointments.
The Discharge Process Needs to be Optimized for Patient Comprehension
To ensure patients have a safe transition from one care setting to the next, an engagement strategy cannot just include intervention within the four walls. The strategy must transcend those boundaries and meet the patient at the point they are at in their care journey. Discharge to home and self-care after discharge is very much part of that journey and can easily turn into an acute care admission if not managed appropriately.
Despite many studies indicating that patients don’t understand or remember important care information provided during discharge, the process has largely gone unchanged. Patients still receive lengthy packets and have a hard time discerning the most important pieces of care information. This is where your patient engagement strategy is paramount. Patients must be prepared for an abrupt change upon discharge. There will no longer be dedicated resources to ensure that they receive the right medication, the right food, and their vitals are monitored. They must be armed with information and able to be active in their own care. For those patients who are unable to care for themselves in the home, a family member or other support person must be identified and educated. Home care resources may need to be allocated.
An effective patient Transition of Care Strategy includes:
- Purposeful Rounding, conducted prior to discharge with focused Transition of Care questions, to uncover where there may be knowledge gaps and help patients understand and internalize the key pieces of information they need to safely move to their next care setting.
- Recorded Discharge Instructions may be offered during the Discharge Process or Transition of Care Round. There is also opportunity to share recorded information specific to the diagnosis and medications prescribed. Ensuring that a patient and their family (as appropriate) is able to receive information beyond just written or spoken at the bedside is essential. This is something that we discuss below.
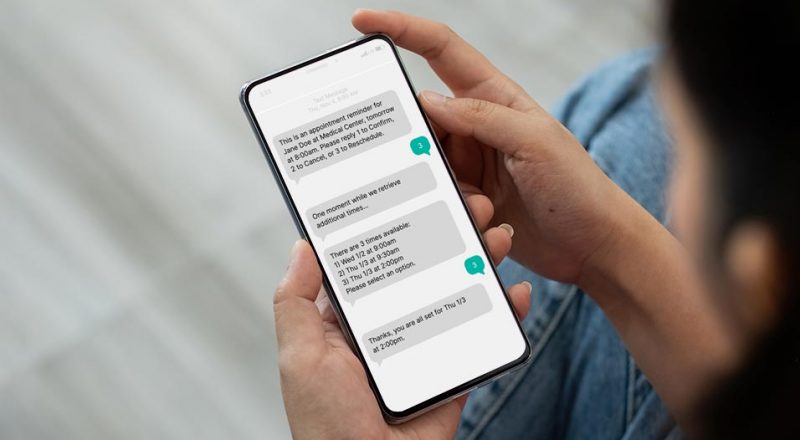
- Timely Post-Discharge Follow-Up allowing patients an opportunity to ask questions and/or request assistance with care needs
Enhanced Care Transitions in Action: The University of Alabama at Birmingham Uses Recorded Care Instructions to Improve Patient Outcomes
In looking to improve care transitions, The University of Alabama at Birmingham (UAB) leadership team saw an opportunity to create a unified experience by engaging patients both inside and outside of the facility. To enable efficient processes and documentation, UAB chose to leverage recorded care instructions to further improve care transitions.
Daily huddles are used to discuss patients due for discharge and those that should receive a discharge round. Using CipherRounds staff member flag the relevant patients and ensure they are prepared for the discharge process. Following the huddle, nurse managers will record 2-3 minute messages for each flagged patient and include information such as numbers to call to schedule follow up and information about medications.
During the discharge process patients are made aware of the recording and told to expect an automated call giving them the opportunity to hear their personalized care recording. Additionally, patients are given a number they or their caregivers can call to access their instructions as often as they’d like.
Utilizing CipherOutreach for care recordings instill confidence in UAB’s patients and gives them the information they need in an easily accessible and understandable format. This innovative approach to engaging patients is what sets the UAB experience apart and has led to a 55% reduction in readmissions over a six-month period.
John Dodd, Program Manager, Office of PX and Engagement at the University of Alabama-Birmingham Health states ,”By collaborating and coordinating care delivery among all those involved in the plan of care, the team is redesigning healthcare to meet patients and family members where they are.”
Care transitions are such a critical part of a patient’s care journey. By creating a cohesive experience driven by proactive engagement, there is immense opportunity to improve outcomes and patient experiences both inside and outside of the facility.
If you are interested in hearing more about the University of Alabama’s experience with recorded care instructions, don’t miss out on their upcoming presentation at this year’s Beryl Patient Experience Conference.