ABSTRACT
There are numerous factors that can impact patients’ understanding of care instructions when transitioning from the hospital setting to home. This retrospective data analysis measured the effect of bundling interventions – a transitional care round and post-discharge outreach call – on patients’ ability to understand information needed to care for themselves safely post discharge. The results showed that patients who received both a transitional care round and a post-discharge outreach call had fewer questions about aspects of their care plan compared to those who only received a post-discharge outreach call. In addition, pairing the two interventions led to the greater likelihood of patients engaging with and completing outreach calls, which is tied to reduced readmissions.
INTRODUCTION
Transitioning a patient from hospital to home is an extremely complex and multifaceted process. Challenges throughout can impact the degree to which patients leave the hospital with an adequate comprehension of their care instructions. This may involve many stakeholders sharing critical pieces of information that can easily be misinterpreted by patients and/or their caregivers.
In addition to the amount of information a patient and family are challenged to absorb regarding new medications, follow-up care, and clinical symptoms, Social Determinants of Health (SDOH) may also play a significant role in a patient’s recovery. SDOH and health literacy are well-documented issues that can affect recovery following an inpatient stay. Furthermore, changes in reimbursement have led to decreased Length of Stay (LOS), which may also impact patients’ time to digest and understand the care plan.
While these issues are not clinical in nature, they can have a profound effect. Although patients may be more comfortable at home with the support of family and friends and away from the stresses of a hospital or post-acute setting, for some, this transition becomes challenging and may result in critical gaps in care.
Some healthcare processes stem from evidence-based bundled interventions, such as a transitional care round and post-discharge outreach call, to reduce the risk of complications and support improved care. Pairing two interventions can help coordinate care and maximize the ability to proactively resolve patient issues.
The purpose of this study was to assess the impact of pairing the transitional care round and outreach call as a way of assessing patient understanding of care instructions as measured by their questions.
THE STUDY
The transitional care round consists of a final review of the personalized discharge plan, including home care needs, durable medical equipment, transportation, follow-up appointments, care instructions, and signs and symptoms to monitor. The post-discharge outreach call confirms that this plan has been effectively carried out and assesses if the patient has remaining questions that can be immediately addressed.
To test this hypothesis, CipherHealth studied the effectiveness of implementing one or both of these complementary strategies: transitional care rounding and post-discharge outreach. A retrospective data analysis was completed of 77 CipherHealth customers, including 484 hospitals located throughout various geographic regions across the United States.
STUDY APPROACH
The analysis included 84,570 patients over approximately 24 months beginning January, 2020. All patients included in the analysis received an outreach phone call after leaving the hospital. During outreach calls, patients were asked a series of medical questions, including understanding of their care instructions and medications, which are known risk factors for readmission. In response, patients could press a button on their keypad to indicate that they had a question, triggering a callback from a care team member to address their concerns and resolve the issues.
A subset of the total population also had a transitional care round conducted during their acute hospital stay and within 24 hours of discharge. During the transitional care round, clinicians asked patients about their understanding of their instructions for home, including symptoms or problems to monitor and an understanding of their medications.
The discharge-related question varied somewhat depending on the health system. For example, a patient might be asked, “Do you feel that we have prepared you to care for yourself and discussed any symptoms or health-related issues you might encounter after leaving the hospital?” Or, in a separate case, “We know you may not be leaving the hospital right now, but do you have any concerns for when you leave? What can we do to help?”
CipherHealth compared the patients’ responses about discharge instructions and medications by comparing patients who received both interventions—transitional care round and post discharge outreach call— to those patients who had only one intervention.
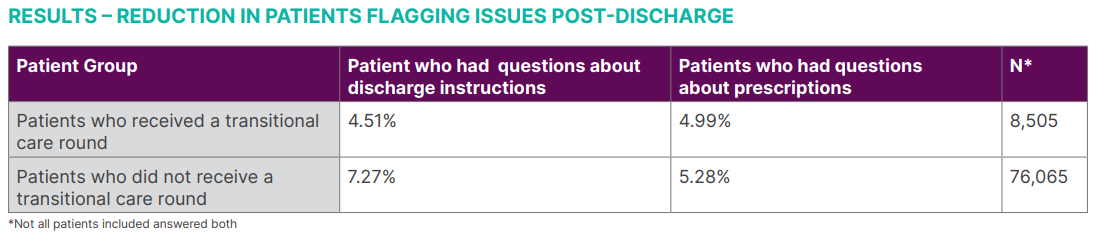
CipherHealth’s analysis found that for patients who received a transitional care round prior to discharge, 4.51% had flagged an issue during the outreach call regarding understanding of discharge instructions, compared to 7.25% who did not receive round prior to discharge. In other words, a lack of transitional care round was correlated with a greater likelihood of patients not understanding their discharge instructions and needing assistance after returning home.
The same was found to be true for patients in regards to obtaining their prescriptions—4.99% of patients who received a transitional care round flagged an issue during the outreach call, compared to 5.28% of patients who did not receive a round prior to discharge. In other words, a lack of transitional care round was correlated with the greater likelihood of patients not obtaining their prescriptions in a timely manner post-discharge.
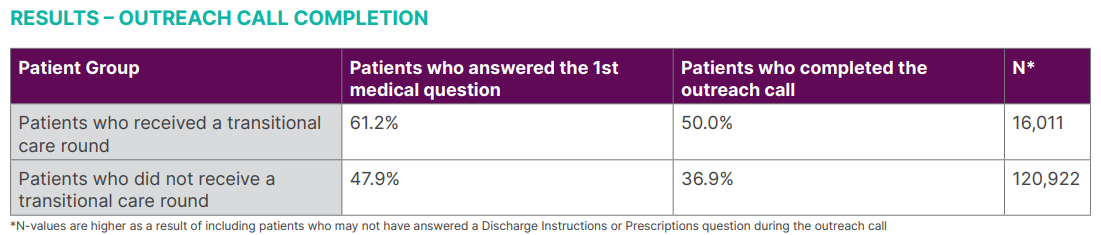
CipherHealth’s analysis identified that for patients who received only an outreach call post discharge, 47.9% answered the first medical question and 36.9% completed the call. In comparison, for patients who received both a transitional care round and an outreach, 61.2% answered the first medical question and 50% completed the call.
This review suggests that supplementing discharge teaching with both a focused transitional care round and post-discharge outreach is an effective way to support a patient’s healing journey. This is especially true as research shows that patients who complete outreach calls readmit less often — the paired process allows patients multiple opportunities to request clarification or additional education from their caregivers and providers, as well as providing patients the necessary time to review and process their discharge instructions.
CONCLUSION
Based on the data in this retrospective study, pairing a transitional care round with an outreach phone call reduces patient questions and leads to increased discharge call completion. The impact of pairing strategies for patients who are transitioning home is thus a recommended, evidence-based approach to effectively care for patients post-discharge and reduce the likelihood of preventable readmissions.