“Depression is a common and treatable mood disorder, and spreading awareness about the different ways those dealing with it can get help could save lives.”—MentalHealthScreening.org

October 5th marks National Depression Screening Day, an event held by hospitals, clinics, colleges, and community groups across the country aimed at increasing education, awareness, and participation in screenings for common mood disorders, such as depression, generalized anxiety disorder, bipolar disorder, and PTSD.
To mark this important event within Mental Illness Awareness Week, and as part of our Behavioral Health Blog Series, CipherHealth wanted to highlight the importance of universal depression screening and connection to treatment.
This is especially critical considering the interplay between comorbid mental health disorders and chronic physical health conditions. According to the National Comorbidity Survey Replication and Robert Wood Johnson Foundation:
25% of adults have a mental health condition
58% of adults have a medical condition
68% of adults with a mental health condition have at least one medical condition
29% of adults with medical conditions have a comorbid mental health condition
The percentage of adults with a mental health condition and at least one medical condition (68%) is striking. Research has indicated that individuals with these comorbidities experience increased symptom burden and functional impairment and a lower quality of life. Individuals with comorbid mental and physical health conditions additionally cost the health care system approximately 300% more than individuals with only a physical health condition/s. Mortality rates for individuals with comorbidity are higher as well; individuals with diabetes, for example, experience a 200% lower mortality compared to individuals with both diabetes and depression.
Treatment for these individuals and the causal pathways between concurrency is often complex. A collaborative care model, however, is a widely effective treatment method for individuals with comorbid mental and physical health conditions. Using a multidisciplinary team lead by a nurse or social work care manager, with support by a consulting psychiatrist and internist, the collaborative care model can:
1. Provide behavioral health care to vastly more patients, and within a primary care setting—both eliminating feelings of stigma associated with going to a mental health provider/clinic and alleviating the burden of needing to go to multiple clinics for treatment
2. Remove healthcare silos and bridge a connection between providers and the delivery of physical and mental health care
3. Help address the behavioral health workforce challenge
Key components to successfully ensuring comorbidities are addressed at a patient-level include administering comprehensive assessments that capture both physical and mental health information, supporting and enabling care coordination activities, and defining and tracking behavioral treatment goals. There is a large role that technology, including CipherHealth’s care management and patient engagement tools, can play in enabling successful collaborative care treatment of behavioral health in primary care.
These include:
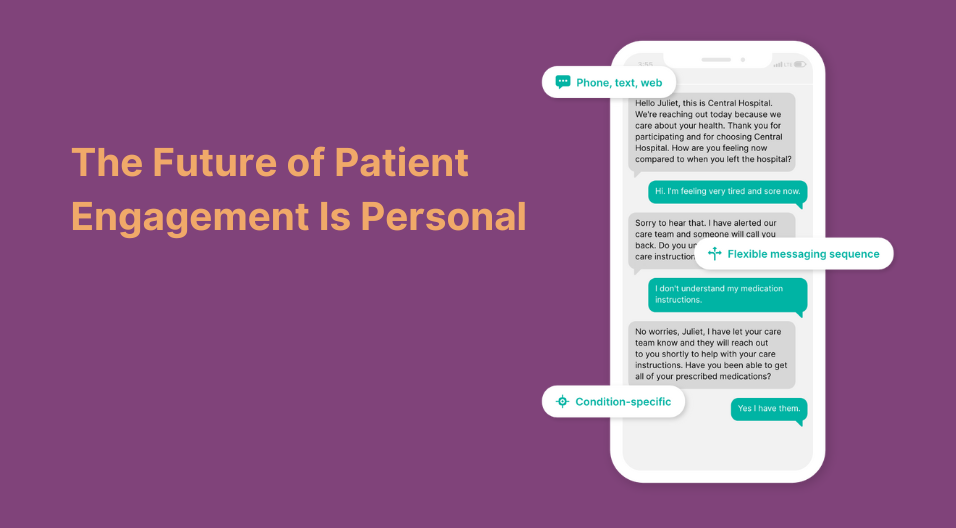
- Incorporating patient facing technology that supports self-management and provides real-time information to care teams
- Enhancing primary care providers’ capacity to treat mild to moderate behavioral health conditions through the provision of education and motivation to patients telephonically or via text
- Incorporating care management tools to ensure the provision of accountable, measurement-based care and standardized screenings
- Conducting tele-psychiatry and tele-evaluations through automated calls or texts, and automated health screenings
Utilizing technology to increase education and awareness, screening rates, and connection to treatment may help clinics successfully implement a collaborative care model and address the needs of the many individuals with concurrent mental and physical health conditions. CipherHealth is proud to work with our many healthcare partners who are working hard to increase their depression screening rates and patients’ access to mental health treatment!