Contributors: Lucia Huang, RN, Nikita Richard, Kamila Berkalieva, MPH, Krisha Patel, MPH, and Lyndsey Lord, MBA, RN
ABSTRACT
With the Hospital Readmission Reduction Program’s focus on reducing 30-day inpatient hospital readmissions, many evidence-based interventions to improve the transition from inpatient to outpatient care have been developed. Compared with inpatient readmissions, less research has focused on emergency department (ED) recidivism, a quality metric increasingly used to measure hospital performance. Successful interventions to reduce 30-day inpatient readmissions may prove to be effective in the ED setting. The objective of this study was to determine the efficacy of post-visit automated calls in reducing ED recidivism.
INTRODUCTION
For many health systems, emergency departments (EDs) function as safety nets for the communities they serve. As the entry point for our most vulnerable patient populations, EDs play an important role in the expansion of care access. With the healthcare industry’s paradigm shift from volume- to value-based care, EDs continue to serve as a barometer for measuring the value of new healthcare delivery models and payment reforms in decreasing cost and improving quality.
ED recidivism is defined as patients returning to the ED for care within a designated time period following an initial ED encounter. As a critical performance measure for emergency medical care, ED revisits are indicators of the quality and safety of care delivery. 1 2 3 Thus, ED recidivism may be considered as a symptom of operational failures during the ED discharge process and in the immediate post-visit follow-up period, with costly implications for healthcare organizations in terms of overall resource utilization.
At the patient level, ED recidivism carries significant clinical implications and is often compounded by a variety of socioeconomic and medical challenges. Return visits to the ED may reflect a lack of comprehension of medication instructions and follow-up care, resulting in the failure of the patient to adhere to the care plan as intended.4 As such, high recidivism rates indicate the need for clinical and community support structures following ED discharge to reduce challenges related to the recent transition home.
Proactive interventions, such as comprehensive discharge planning and purposeful telephonic follow-up, have been studied extensively and are demonstrated to be effective in reducing inpatient readmissions.5 6 7 8 We hypothesize that these interventions can be expanded to the emergency department in an effort to improve the delivery of high-quality care across the entire continuum of admission. The objective of this study is to assess the impact of post-visit automated calls in reducing the risk of avoidable ED revisits.
METHODS
CipherHealth conducted a retrospective analysis using emergency department utilization data at a client organization, Sturdy Memorial Hospital (“Sturdy”) in Attleboro, MA. The study population was comprised of individuals enrolled in the automated post-ED visit outreach call program from September 2017 to August 2018, which consisted of all patients discharged from the emergency department at Sturdy during this timeframe.
The automated call program was utilized to deliver information to clinicians regarding the patient’s condition following discharge. The call program consisted of one automated phone call 48 hours post-visit, with six questions assessing general health status, medications, care team communication, follow-up care, and discharge instructions. These areas of focus were determined in collaboration with CipherHealth and ED clinician leaders at Sturdy, and align with clinically-validated best practice guidelines published by CipherHealth. Patients indicated their responses using the touch-tones on their landline and/or mobile phones. If patients responded negatively to a question, ED nurses received an automatic alert and were immediately notified to manually call the patient back and resolve the issue.
To maximize compliance, patients were notified by the Sturdy nursing staff during the discharge process that they would receive a call within the next 48 hours. In addition, the automated calls utilized voice talent reflecting the regional accent. In the event of a missed call, the patient received a voicemail explaining that another attempt would be made in the near future.
Patient response data was delivered via an outcomes reporting dashboard. Prior to analysis, all identifying data such as name, date of birth, and medical record number were removed.
RESULTS
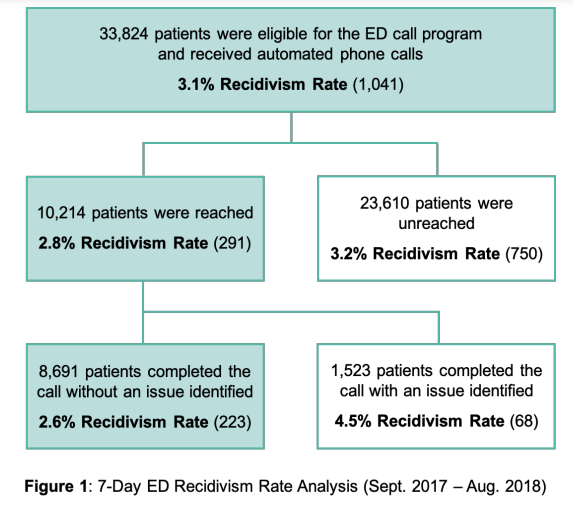
Patients who were reached by the call had an 11% lower likelihood of returning to the ED within 7 days of initial discharge as compared to those who were not reached, with odds found to be marginally significant (OR = 0.89, 90% CI (0.8, 1.0)). Of the 33,824 patients selected for the study, a total of 1,041 (3.1%) returned to the ED within a 7-day period. The outcomes for different patient groups are summarized in Figure 1. The recidivism rate among patients who answered the general status question (10,214) was 2.8% as compared to 3.2% for those who did not answer the question (23,610).
Patients who identified an issue on the call were 1.78 times more likely to require hospital admission, compared with those who did not identify any issues on the call (OR = 1.78, 95% CI (1.35, 2.34)). Responses to the general status question (“How are you feeling now compared to when you were released from the emergency room?”) yielded the highest correlation with ED recidivism of the six questions in the automated call. Patients who responded negatively to the general status question had a 6.4% recidivism rate, as compared to 4.3% and 4% for questions focused on medication and discharge instructions, respectively.
CONCLUSION
As is the case with inpatient hospital readmissions, emergency department recidivism is frustrating and costly for patients and providers alike.9 This study suggests that automated post-visit calls can serve as an effective strategy in reducing ED recidivism, thereby improving care coordination as patients navigate the transition from one care setting to the next. Furthermore, using self assessment through automated phone calls can identify patients who are at a high risk of returning to the ED. Interventions targeting 30-day hospital readmissions may be utilized across the patient care journey, including the ED, to effectively maintain health outcomes and prevent potential adverse events. To further assess impact, future research should focus on the relationship between proactive follow up strategies and healthcare utilization trends across the continuum of care.
REFERENCES
1. Pham, J., Kirsch, T., Hill, P., DeRuggerio, K., & Hoffmann, B. (2011). Seventy-two hour returns may not be a good indicator of safety in the emergency
department: A national study. Academic Emergency Medicine, 18(4): 390-7.
doi: 10.1111/j.1553-2712.2011.01042.x
2. Lindsay, P., Schull, M., Bronskill, S., & Anderson, G. (2002). The development of indicators to measure the quality of clinical care in emergency departments following a modified delphi approach. Academic Emergency Medicine,
9(11): 1131-9. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12414461
3. Schenkel, S. (2000). Promoting patient safety and preventing medical error
in emergency departments. Academic Emergency Medicine, 7(11): 1204-22.
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11073469
4. Griffey, R., Kennedy, S., D’Agostino McGowan, L., Goodman, M., & Kaphingst, K. (2014). Is low health literacy associated with increased emergency department utilization and recidivism? Academic Emergency Medicine,
21(10): 1109-15. doi: 10.1111/acem.12476
5. Misky, G., Wald, H., & Coleman, E. (2010). Post-hospitalization transitions:
Examining the effects of timing of primary care provider follow-up. Journal of
Hospital Medicine, 5(7): 392-7. doi: 10.1002/jhm.666
6. Kansagara, D., Ramsay, R., Labby, D., & Saha, S. (2012). Post-discharge
intervention in vulnerable, chronically ill patients. Journal of Hospital Medicine,
7(2): 124-30. doi: 10.1002/jhm.941
7. Inouye, S., Bouras, V., Shouldis, E., Johnstone, A., Silverzweig, Z., & Kosuri,
P. (2015). Predicting readmission of heart failure patients using automated follow-up calls. BMC Medical Informatics and Decision Making, 15(22). Retrieved
from https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-015-0144-8
8. Harrison, P., Hara, P., Pope, J., Young, M., & Rula, Z. (2011). The impact of
postdischarge telephonic follow-up on hospital readmissions. Journal of Population Health Management, 14(1): 27-32. doi: 10.1089/pop.2009.0076
9. Boutwell, A., Johnson, M., Rutherford, P., Watson, R., Vecchioni, N., Auerbach, B., Griswold, P., Noga, P., & Wagner, C. (2011). An early look at a fourstate initiative to reduce avoidable hospital readmissions. Health Affairs, 30(7):
1272-80. doi: 10.1377/hlthaff.2011.0111