

Key Predictors of Readmission in Inpatient and High-Risk Patient Populations
Issues triggered on CipherHealth post-discharge outreach calls at Middlesex Hospital are key leading indicators of future readmissions
Background
Middlesex Hospital is an approximately 300-bed acute care community hospital located in Middletown, CT. An early adopter of CipherHealth’s solutions, they implemented Post-Discharge Communications for all inpatients, including their CHF (Chronic heart failure) and COPD (Chronic obstructive pulmonary disease) programs, to best support patients post-discharge and intervene quickly should patients indicate they need assistance. CipherHealth’s analysis shows that issues triggered on Middlesex Hospital’s Care Calls were strong predictors of future readmissions. In particular, difficulty understanding discharge instructions and arranging transportation to follow-up appointments were strongly linked to future readmission.
Challenges
High-risk patients often have chronic conditions and are more expensive patients. It is in all health systems’ financial best interest to reduce readmissions and, moreover, it is better for the patient. If Middlesex could predict who would likely need to be readmitted to their inpatient, CHF or COPD programs, they could intervene with a follow-up call and provide support and resources to this subset of patients, prevent readmissions and earn more favorable reimbursement from CMS (Centers for Medicare & Medicaid Service) and commercial payers.

Goal
In all three programs — Inpatient, CHF and COPD — Middlesex wanted to provide personalized support and resources to those patients experiencing difficulties post-discharge. “When patients leave the hospital, we want to make sure they have that touch point,” Elizabeth DePierro, Readmission Program Manager, Quality Improvement, CPHQ, said. Using automated outreach, they could focus on those patients who flagged an issue. Since difficulty understanding discharge instructions and arranging transportation to follow-up appointments were strongly linked to future readmission, they could intervene early and provide support. This would go a long way towards preventing readmission and lowering associated costs.
Middlesex Hospital also wanted to address underlying social determinants of health. In many cases, their patients could not afford their medications or did not have access
to transportation to get to their follow-up appointments, as well as other roadblocks to getting the care they need. “The main thing is that those patients get connected with the right services in the community,” DePierro said of the need for post-discharge outreach.
Impact
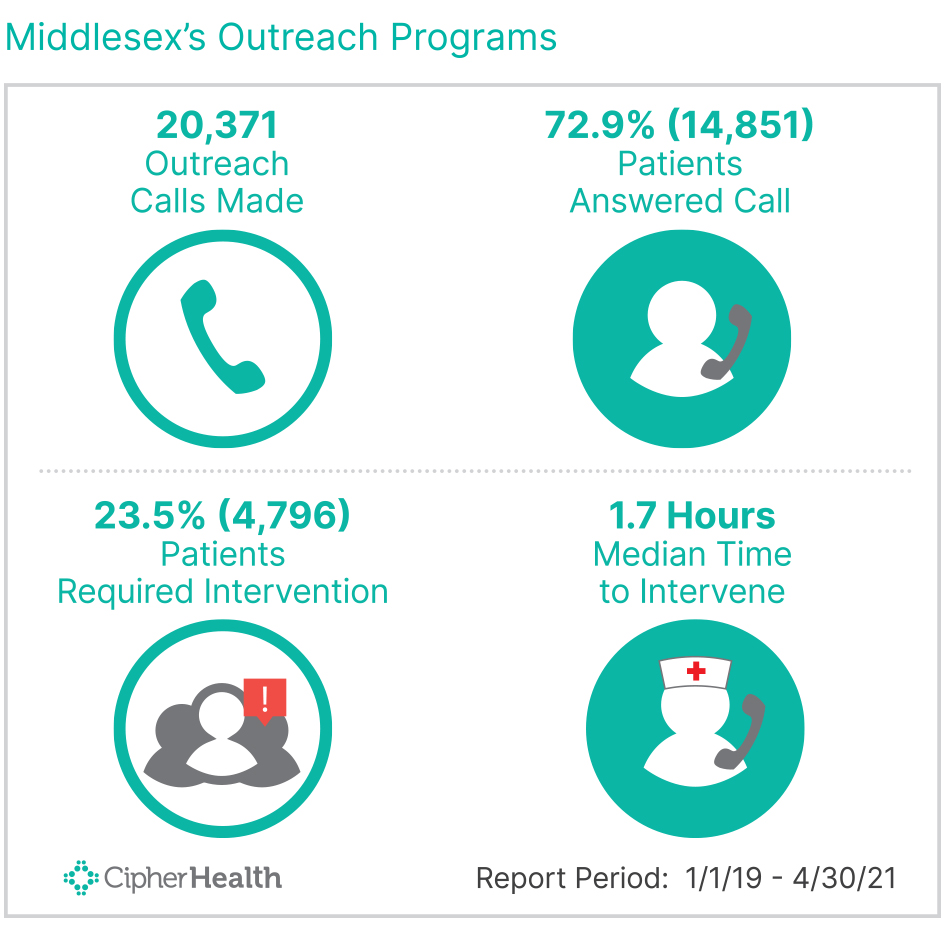
Between January 2019 and May 2021, Middlesex’s Outreach programs called 20,371 patients, preventing an estimated 120 readmissions.
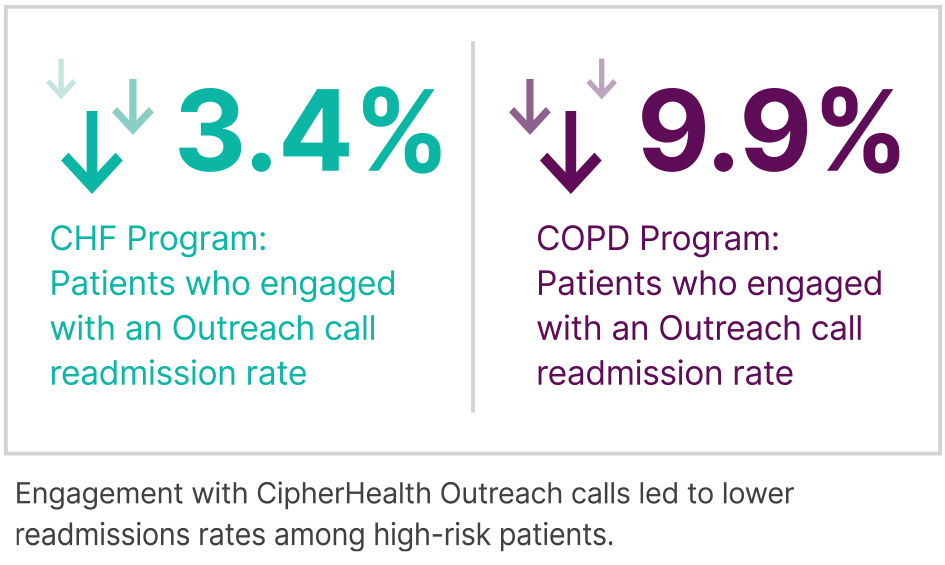
The results were especially noteworthy for their CHF and COPD programs — those patients who engaged with an Outreach call were readmitted at rates that were 3.4% and 9.9% lower, respectively, than patients who did not engage.
In addition, it was instructive to examine what kind of issues triggered on an Outreach call could predict readmissions by cohort:
- For inpatients, the readmissions rate was highest — 17.2% — when patients reported they felt worse since leaving the hospital.
- For CHF patients, the readmissions rate was highest — 28.3% — when patients reported that they had questions about their discharge instructions.
- For COPD patients, the readmissions rate was highest — 29.1% — for patients who responded they didn’t have transportation for their follow-up appointment.
When patients flag issues, such as the above, Outreach calls are strong predictors of future readmissions. Middlesex focused follow-up time and resources on patients who triggered specific issues.
Conclusion
Middlesex’s success with CipherHealth’s Post-Discharge Communications serves as a model for larger healthcare systems looking to gain more insight into key indicators of readmissions for their overall and high-risk patient populations. The ability to predict who will likely be readmitted is not only in health systems’ financial best interest but also allows their staff to intervene in time to improve clinical outcomes for their patients.




