The mandatory team TEAM model is rolling out 2026 and health systems will be held accountable for both cost and quality across entire surgical episodes, from admission through 30 days post-discharge.
Here’s how a patient-facing OS can help you meet those requirements and improve clinical outcomes at every step.
Success under TEAM depends on start-to-finish coordination
Avoiding readmissions is just the start. TEAM quality scores also include safety events like infections, falls and pressure injuries, along with patient experience metrics like HCAHPS.
To strengthen financial performance under TEAM, healthcare leaders are turning to digital tools that go beyond what the EHR can do on its own.
CipherHealth’s patient-facing OS supports the full care journey. It brings together Rounding, Outreach and Self-Service tools to close gaps, prevent harm and keep patients engaged from start to finish.
#1 Set your standard across all units and staff
Preventing safety events starts with consistent, high-quality rounding. When every unit follows the same evidence-based workflows, staff know what to check, what to ask and when to escalate. This reduces variation and ensures patients receive the same standard of care, no matter the shift, department, or facility.
Just as important, staff have a reliable process designed around their needs that just works every time.
#2 Give teams real-time service recovery opportunities
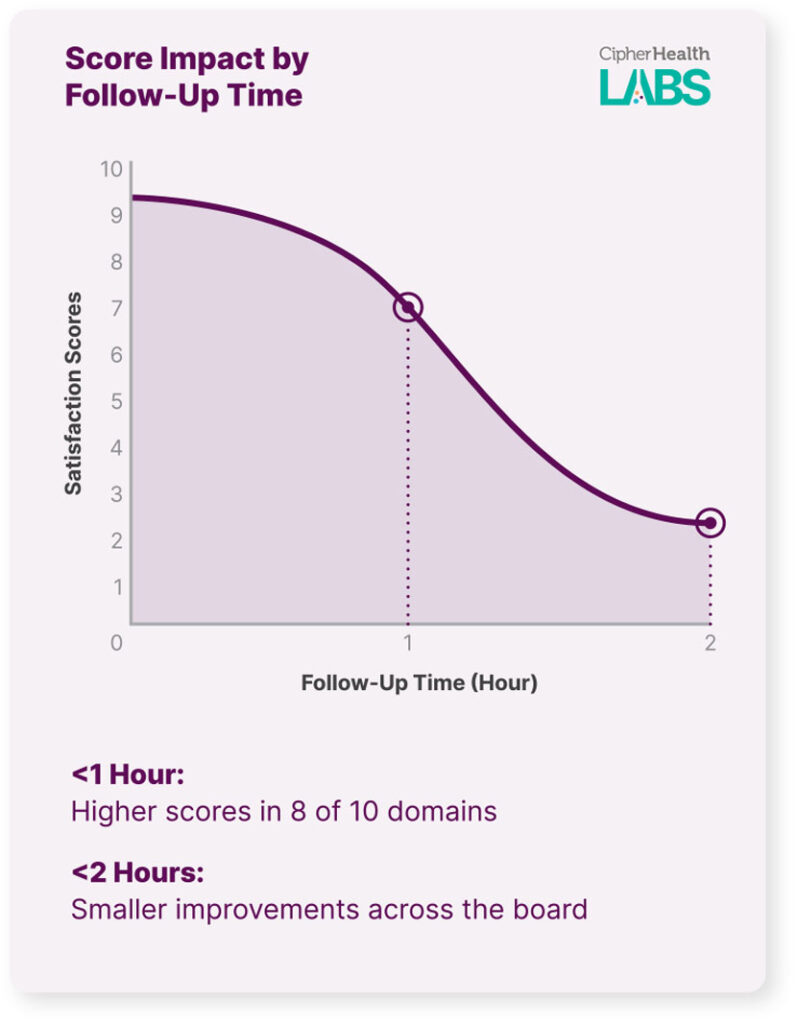
Care teams need timely, actionable insights that help them respond in the moment.
Real-time data from rounding and outreach gives staff the visibility they need to spot risks, escalate issues and make quick adjustments. That kind of responsiveness helps teams stay aligned with TEAM expectations and avoid costly gaps in care.
As we continue to see, timeliness on patient-reported issues is a key factor in improving clinical outcomes as well as patient experiences.
#3 Engage patients post-discharge to catch complications early
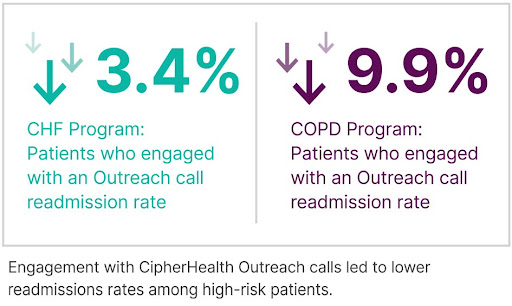
For high-risk patients, what happens after discharge can be just as important as the hospital stay itself. Follow-up needs to be timely and personalized. Instead of relying on disjointed manual processes, automated outreach gives teams a faster way to identify concerns and intervene before complications lead to readmissions.
Indeed, Middlesex Hospital reduced readmissions by 3.4% for CHF and 9.9% for COPD patients using CipherHealth. By identifying key risk factors, like confusion about discharge instructions and lack of transportation, they prevented an estimated 120 readmissions.
#4 Surface patient needs directly through self-service tools
As patients wait in the ED or recover on the unit, self-service tools let them easily share concerns or requests in real time. They can access the site from any device using a QR code or a link sent via text. That input goes straight to the care team, helping them respond quickly, prioritize tasks, and improve the patient experience while giving patients more control.
#5 Monitor safety, satisfaction and readmissions with integrated analytics
Tracking TEAM performance shouldn’t require toggling between tools or chasing down reports. When rounding data, outreach insights and patient feedback live in one place, and are summarized to help focus on the right issues, it’s easy to spot trends, act decisively and continuously improve outcomes over time.
A patient-facing OS is your strategic advantage
To succeed under TEAM and other value-based care models, hospitals must move beyond siloed systems, manual workarounds, and EHR-only tools. The financial risk is too great.
CipherHealth connects every touchpoint, from pre-visit prep and rounding to follow-up and long-term monitoring, so each experience feels familiar, personalized, and coordinated.
By unifying engagement across the care journey, a patient-facing OS helps you meet TEAM requirements with less guesswork and more consistency. The result? Fewer readmissions, safer care, and a stronger path to financial performance.