This is part two of a blog series entitled “Revisiting MACRA;” see parts one and three. We also invite you to check out this free guide called “Leveraging Automated Outreach to Succeed in MACRA.”
Gone are the days when the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) was thought of as an abstract regulatory framework that physicians can put off paying attention to until tomorrow. With the performance year coming to a close, participating providers will soon be more on the hook for reporting data that will impact Medicare payments.
As discussed in the first part of this series, the vast majority of eligible physicians will qualify for the Merit-based Incentive Payment System (MIPS) path. This installment focuses on the performance measures associated with the program, and how participants can leverage patient engagement strategies to succeed with MIPS reporting.
Boosting MIPS Performance Across Four Categories
MIPS replaces and consolidates several programs, including the Physician Quality Reporting System (PQRS), Medicare EHR Incentive Program or “Meaningful Use,” and Physician Value-Based Payment Modifier (VBM). Its goal is to tie payments to quality and efficient care delivery, drive improvements in care processes and outcomes, increase the use of healthcare information, and lower costs.
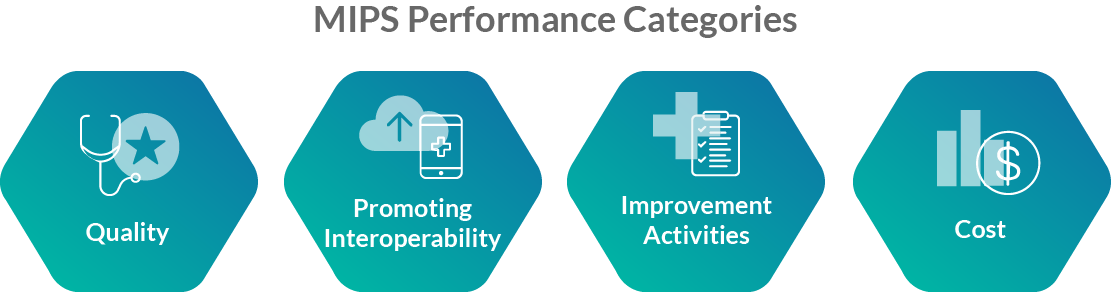
MIPS performance is evaluated based on data reported by clinicians across four categories – Quality, Promoting Interoperability, Improvement Activities, and Cost. Each category is weighted differently and consists of various measures that participants can choose to report on over a 12-month performance period, which impacts payment adjustments two years later (e.g., data reported in 2019 determines financial incentives or penalties in 2021).
One way for medical groups to help bolster MIPS performance in each of the four categories is to develop and implement a scalable patient outreach strategy.
PQRS Is Replaced By The Quality Category
The Quality category replaces PQRS and is the most heavily weighted of the four. It’s comprised of 275 quality measures that allow clinicians to report data most relevant to their specialty and patient population. The measures assess quality in a variety of ways and are broken down by type, including “Efficiency,” “Outcome,” “Process,” “Structure,” and “Patient Engagement Experience.” Patient engagement solutions, such as outreach, can help drive high performance in this category.
For example, a number of measures center on preventive health services, such as “Colorectal Cancer Screening,” “Influenza Immunization,” and “Diabetic Foot and Ankle Care, Peripheral Neuropathy – Neurological Evaluation.” Automated reminders by way of phone, text message, and/or email is a proven method for increasing the likelihood of patients coming in for screenings and vaccinations. They’re also an effective way of closing gaps in care for patients managing chronic conditions and keeping them engaged with their health.
There are a number of other examples of how patient engagement tools can be used to support the various quality measures. In order for providers to determine the right patient engagement strategy, it’s important to first identify the quality measures that make the best sense for their practice.
Reporting Against The Promoting Interoperability Category
The Promoting Interoperability category, formerly known as Advancing Care Information, seeks to promote patient engagement and electronic exchange of information using certified electronic health record technology (CEHRT). This replaces the aforementioned “Meaningful Use” program. Providers must use a CEHRT in order to score in this category, and there are two sets of measures that correspond to the applicable CEHRT edition.
For this category, participants are required to report on a number of base measures, which capture the degree to which physicians are using their CEHRT to transmit and receive patients’ summary of care to facilitate care transitions, provide patient access to health information, and e-prescribe. Once the base score requirements are met, there are additional performance measures that can help improve results.
For example, the “Patient-Specific Education” measure can be satisfied when providers use a CEHRT-integrated care management platform to provide patients electronic access to relevant educational content. Clinicians can also build on their score by communicating with patients via secure messaging channels or reporting immunization data to public health agencies using a CEHRT.
Improvement Activities Category As A Measure Of Effort Invested In Enhancing Care
The purpose of the Improvement Activities category is to gauge the extent to which physicians are engaging in activities to improve clinical practice. Similar to the Quality category, Improvement Activities consists of a list of 113 measures that providers can choose from. These measures are broken down into subcategories, including “Beneficiary Engagement,” “Care Coordination,” and “Population Management,” amongst others.
There are many patient engagement tools that can be leveraged to enhance Improvement Activity measures. Examples include automated reminders, which can be leveraged for measures such as “Improved Practices that Engage Patients Pre-Visit” and “Chronic Care and Preventative Care Management for Empaneled Patients;” or post-visit text messages that provide patients access to satisfaction surveys for the “Collection and Follow-Up On Patient Experience and Satisfaction Data On Beneficiary Engagement” measure.
It’s also worth noting that providers that participate in a certified patient-centered medical home (PCMH), such as the National Committee of Quality Assurance PCMH program, earn full credit for the Improvement Activities category by attesting to it during the submission period.
Cost Category Focuses On Avoidable Healthcare Utilization
The Cost category differs from the others because it’s calculated automatically from CMS claims data. Specifically, the score is derived from two measures: “Medicare Spending per Beneficiary” and “Total Per Capita Costs.” Due to the fact that providers are not given the option to pick and choose which measures to target, they must focus on maximizing overall cost efficiency of care delivery. One way to do this is by proactively mitigating avoidable utilization of healthcare services, especially with respect to patients managing chronic conditions.
Patient engagement technology can play a key role in helping to reduce preventable healthcare costs. For example, an outreach solution can be used to engage patients post-discharge from an inpatient setting to schedule a visit with an outpatient provider, or in between appointments to remind them of upcoming visits and gauge health literacy.
A Path Forward
The patient engagement strategies presented herein are several among many that can help improve MIPS performance. It’s important to remember that each group practice is different and serves a unique patient population, and as such there is no single mix of strategies to guarantee success. Medical groups that take a systemic approach to patient engagement and consider how practice adjustments impact not just MIPS reporting, but other aspects of their organization, will likely see the best results.
With that being said, for medical groups just beginning to think about technology improvements in anticipation of MIPS, patient outreach is a great place to start. Outreach, including appointment reminders, preventive outreach, and post-visit follow-up, can help enhance performance in each of the four reporting categories and position providers for clinical and operational success.
CipherHealth’s single platform offers medical groups many of the patient outreach solutions discussed in this article. To see how our technology can help improve your MIPS reporting, click here to request a demo.