6,406
Patients Called
84%
Answered Clinical Question
43%
Patients Required Intervention

Achieving $15M in Savings by Reducing Readmissions With Post-Discharge Follow-Up
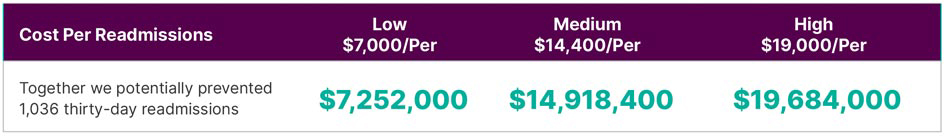
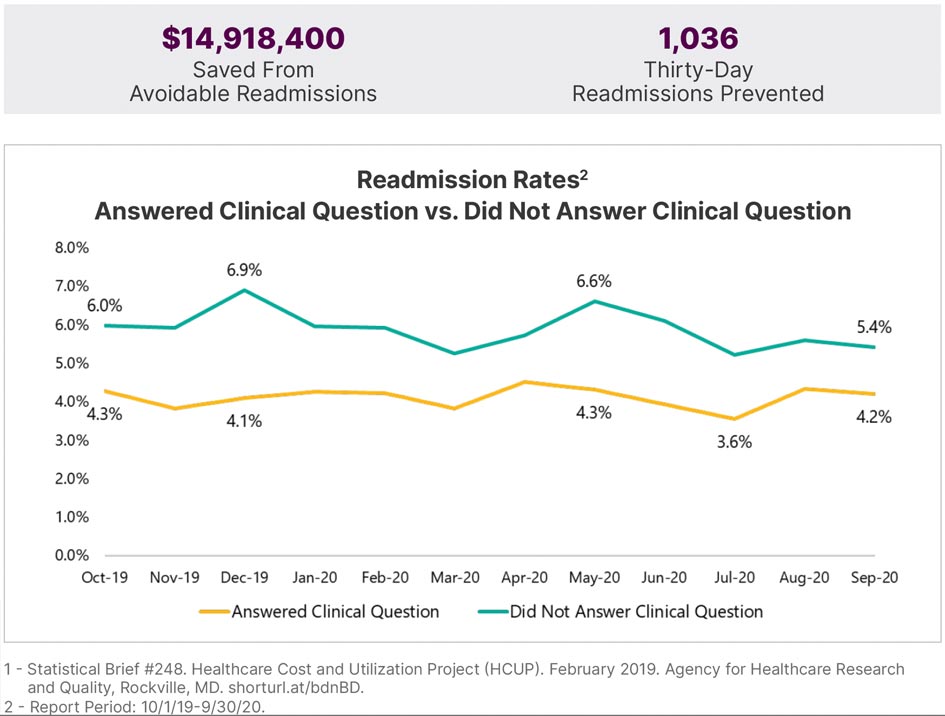
Preventing readmissions is what’s important to us, and we had just under $15M in savings with doing these post-discharge follow-up calls. We’re not spending near that amount to provide these services, and they are making a huge difference. It results in patient satisfaction, lower readmission rates, and it does have a significant financial impact in our organization.
6,406
Patients Called
84%
Answered Clinical Question
43%
Patients Required Intervention
BACKGROUND
The team at Intermountain Healthcare was focused on addressing clinical issues like making sure patients understood discharge instructions, were able to obtain their prescriptions and had no questions about their medications. To improve the patient experience, they implemented a Post Discharge Follow-Up program and staffed its call-back team with experienced nurses. As a result, Intermountain saw dramatic improvements in its readmission rates and related cost savings.
Financial Impact of Readmissions Prevented1