Patient Engagement Platform
Understand every patient with a single solution
3 ways to stand out with CipherHealth
Get flexible
solutions
Leverage patient engagement solutions that reach patients at scale – and grow with you as your patient communications needs evolve.
Manage at-risk
patients
Enroll patients in engagement programs, from chronic condition management to annual wellness visits.
Optimize healthcare staff efficiency
Report and
analyze
Reduce IT
burden
Consolidate healthcare organization vendors with a single-source provider for patient engagement solutions for all stages of patient care.
Future-proof your
investment
Maximize your patient engagement initiatives with a healthcare solution expressly built for patient activation and communications.
Optimize patient, staff and caregiver communications with a purpose-built patient engagement platform

Community Health Network
reduced readmission rates by 32% across inpatient and ED programs
Dr. Patrick McGill
EVP & Chief Analytics Officer
Community Health Network
Allow your IT team to be more efficient and maximize workflows with a flexible, scalable patient engagement technology.
Maximize your EHR investment with integrations that improve message deliverability rates, drive patient portal activations and allow for vendor consolidation.
Leverage our clinical team and implementation experts to establish best practices.
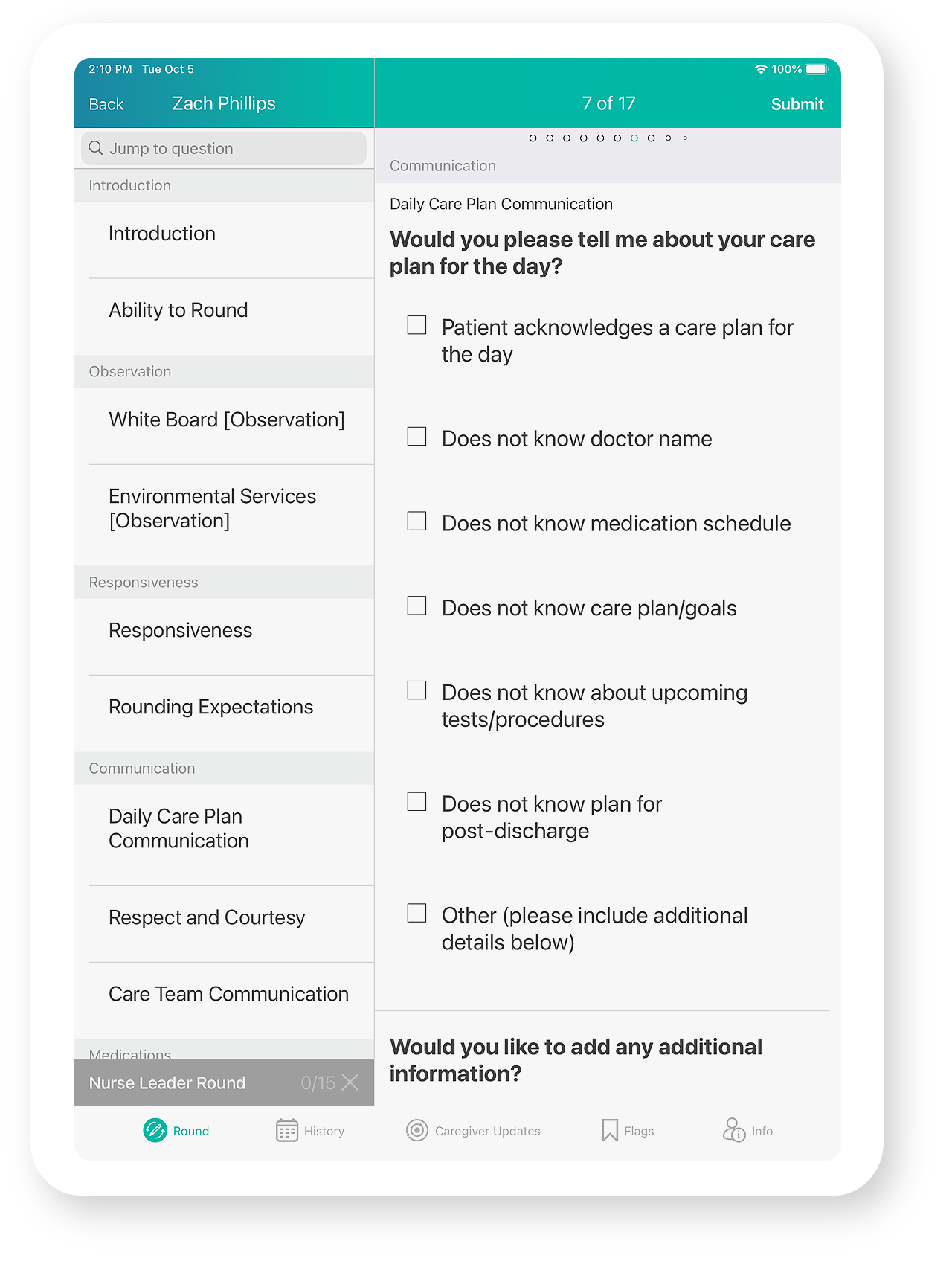
Meet the adherence requirements set forth by HITRUST for securely managing data, information risk, and compliance.
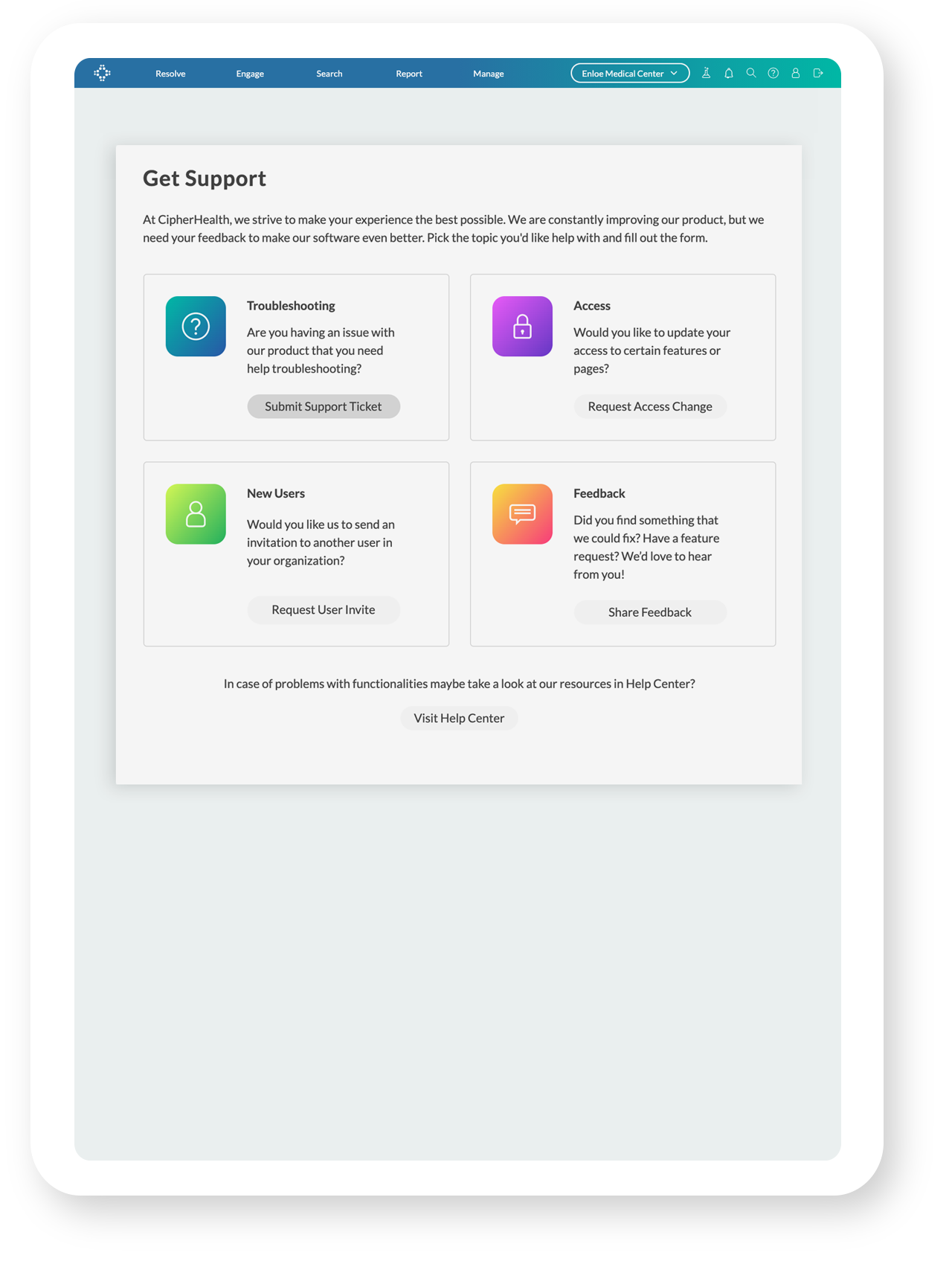
Connect with our support team, change features access and add new users in real-time directly within the app for a superior support experience.
Engaged in nearly
Interacted with
nearly 2.5% of the US population
Close care gaps, improve staff satisfaction and achieve financial goals today








